Pharmaceutical regulatory compliance is a critical and growing part of the industry. The U.S. pharmaceutical regulatory affairs market is expected to reach over $2.4 billion by 2030, growing steadily at nearly 8% annually from 2024.
This growth highlights how important it is for pharmaceutical companies to manage compliance, both to meet strict safety standards and to keep pace with changing regulations.
In this blog, we’ll explain pharmaceutical compliance, why it matters, and the challenges companies face. We’ll also cover how to manage compliance effectively in this demanding environment.
What is Regulatory Compliance in the Pharmaceutical Industry?
Regulatory compliance means adhering to the legal, ethical, and quality standards set by national and international authorities throughout the drug lifecycle. This includes everything from research and clinical trials to manufacturing, distribution, and post-market monitoring.
These regulations have been shaped over many years through scientific study, public health priorities, and experiences with past safety issues. Adhering to them helps ensure that pharmaceutical products remain safe, effective, and meet quality standards no matter where they are produced or distributed.
Importance of Regulatory Compliance
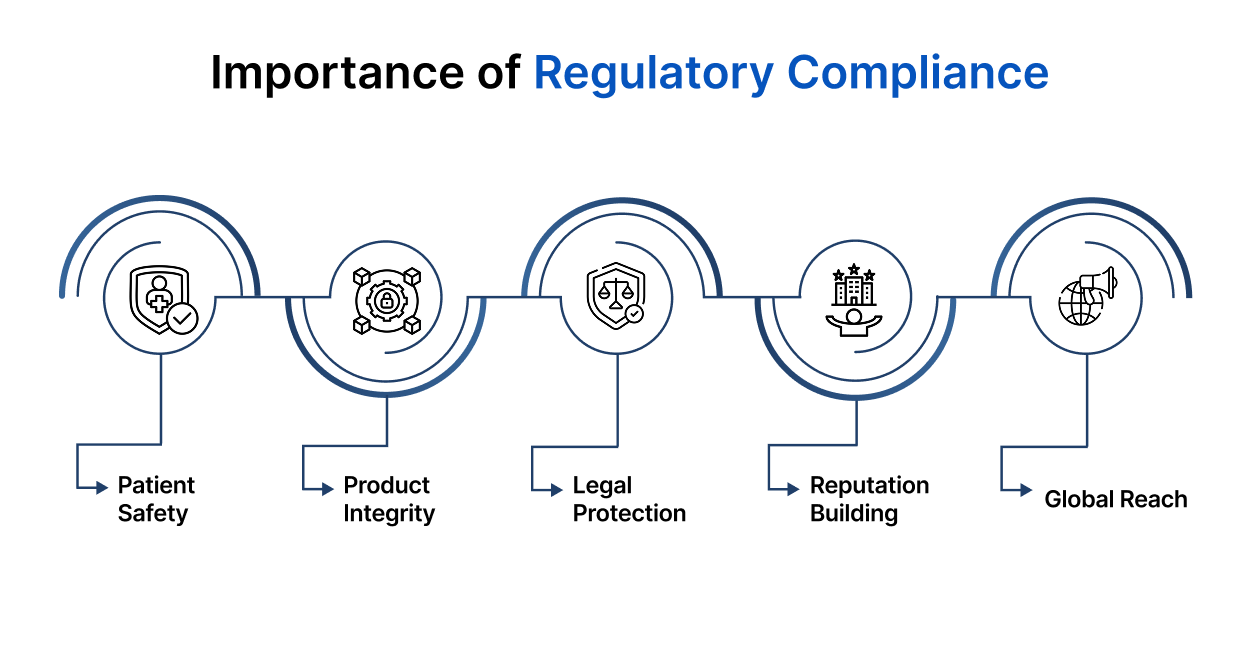
- Protects Patient Safety: Regulations help prevent issues like contamination, incorrect dosages, or adverse reactions by requiring strict quality controls at every stage.
- Keeps Products Effective Medications are tested thoroughly to confirm that they work as intended and continue to do so throughout their shelf life.
- Prevents Legal and Financial Consequences: Failure to follow rules can result in recalls, bans, fines, or even legal action against the company.
- Builds Public Trust and Reputation: Meeting compliance boosts a company’s reputation with regulators, doctors, and the public.
- Enables Market Access and Global Distribution: Compliance is needed to get approval to sell drugs worldwide. Without compliance, medicines cannot make it to patients.
Knowing why compliance is important is just the beginning; understanding which organizations set these standards and the rules companies need to follow is equally essential.
Key Regulatory Bodies and Standards
Pharmaceutical compliance is overseen by both national and international regulatory authorities. Every regulatory agency sets rules to make sure medications are safe, effective, and high in quality. For pharmaceutical companies, understanding these agencies and their standards is essential.
Major Regulatory Bodies
- U.S. Food and Drug Administration (FDA): The FDA oversees the approval and monitoring of pharmaceutical products in the United States, with regulations like 21 CFR Part 210/211 (for manufacturing) and 21 CFR Part 11 (for electronic records and signatures). It plays a critical role in clinical trial approvals, labeling, marketing compliance, and post-market surveillance.
- Health Canada: Through its Health Products and Food Branch (HPFB), Health Canada regulates pharmaceuticals, ensuring they meet Canadian standards for safety, efficacy, and quality.
- European Medicines Agency (EMA): The EMA evaluates medicinal products for use across EU member states. It promotes the harmonisation of safety and efficacy standards through the centralised authorisation procedure, ensuring consistency across the region.
Other important agencies include the Therapeutic Goods Administration (TGA) in Australia and the Medicines and Healthcare products Regulatory Agency (MHRA) in the UK. These organizations adapt global standards to their regions and enforce compliance.
Core Standards and Guidelines
- HIPAA (Health Insurance Portability and Accountability Act) sets rules for protecting patient data privacy in the U.S., impacting pharmaceutical companies that handle sensitive health information.
- U.S. Federal Code Title 21, Part 11 sets rules for electronic records and signatures, making sure digital documents in pharmaceutical processes are secure and reliable.
Together, these regulatory bodies and standards form a complete framework that pharmaceutical companies must follow to guarantee their products are safe, effective, and compliant with laws around the world.
Components of Regulatory Compliance
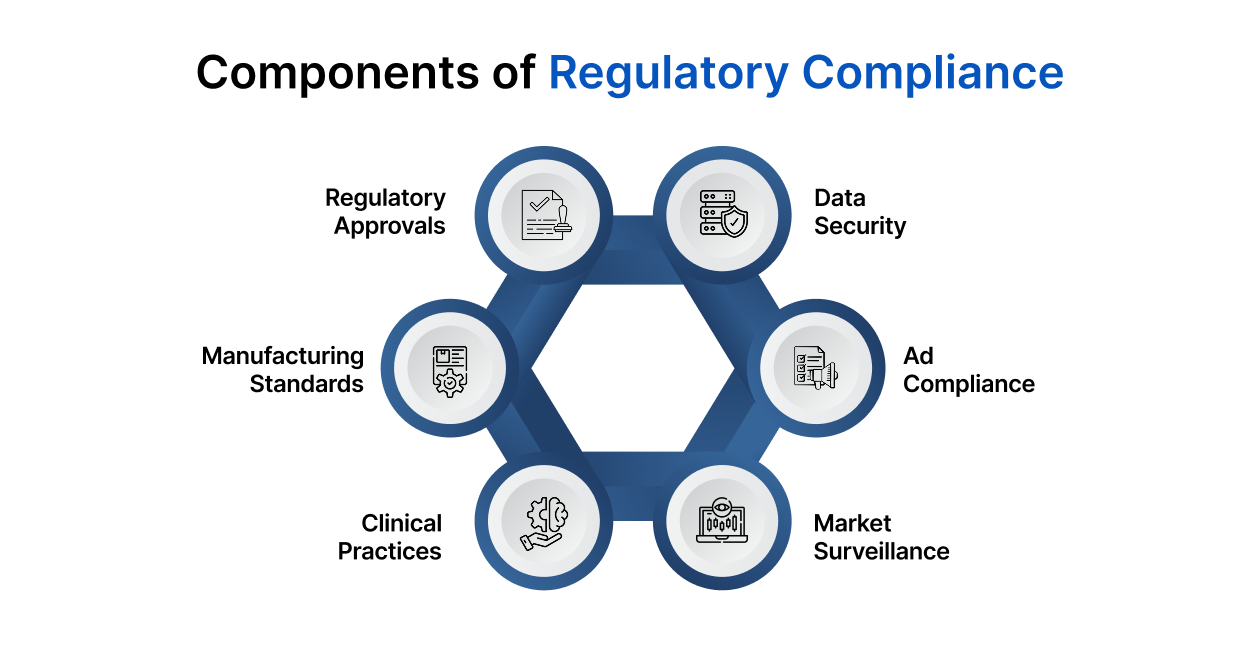
Pharmaceutical compliance spans a drug’s entire lifecycle. Each step is designed to uphold legal requirements while ensuring patient well-being and product reliability.
1. Regulatory Submissions and Approvals
Before a drug reaches the market, it undergoes a thorough review. Regulatory bodies check for safety, effectiveness, and quality before giving the green light. This includes:
- Investigational New Drug (IND) Applications: Filed before clinical trials, sharing early research and plans for human testing.
- New Drug Applications (NDA) and Abbreviated New Drug Applications (ANDA): Submitted for approval of new drugs or generics, providing evidence of clinical trial results, manufacturing processes, and proposed labeling.
- Marketing Authorisation Applications (MAA): For obtaining marketing approval in specific regions, such as the EU.
2. Good Manufacturing Practices (GMP)
GMP refers to a set of regulations and guidelines governing the production of pharmaceutical products. These standards ensure that products are produced consistently and controlled to the highest quality standards.
Key aspects include:
- Raw Material Quality: Confirming that all materials used in production meet quality standards.
- Facility Conditions: Production areas must meet cleanliness and safety benchmarks.
- Production Processes: Every step in the process must be documented and verified to ensure consistent outcomes.
3. Good Clinical Practices (GCP)
GCP ensures clinical trials are conducted ethically and that the data collected is trustworthy. It includes:
- Informed Consent: Participants must clearly understand the trial and voluntarily agree to join.
- Trial Design: Studies must follow detailed, well-documented protocols.
- Data Management: All trial data must be accurate, complete, and traceable.
4. Post-Market Surveillance and Pharmacovigilance
Compliance doesn’t stop once a drug is approved. Companies need systems in place to monitor performance and catch any issues early.
- Adverse Event Reporting: Any negative reactions must be reported to authorities.
- Risk Management: Plans should be in place to handle known risks.
- Product Recalls: Companies must be ready to act fast if something goes wrong.
5. Labeling and Advertising Compliance
Regulations ensure marketing claims are fair and truthful. This applies to materials shared with healthcare professionals and consumers alike.
This includes:
- Product Labeling: Should clearly outline how to use the drug, possible side effects, storage instructions, and other important details.
- Advertising Standards: Pharmaceutical marketing must follow regulations, such as the FDA’s OPDP in the U.S. and EMA guidelines in Europe, to ensure all claims are backed by scientific proof.
6. Data Integrity and Security
As more processes go digital, maintaining trustworthy records becomes essential. Regulations like 21 CFR Part 11 (U.S.) and Annex 11 (EU) guide how digital systems are managed.
- Change Tracking: Every modification must be logged and attributed.
- Security Measures: Systems must guard sensitive data from unauthorized access.
- System Validation: Electronic tools must be tested and proven reliable.
Together, these components not only protect public health but also support innovation by keeping systems transparent and dependable.
Challenges in Maintaining Regulatory Compliance
Staying compliant isn’t always simple. It takes ongoing effort and resources to keep up with shifting expectations and market demands.
1. Complex and Changing Regulatory Requirements
As science advances, so do regulations. New therapies like biologics or personalized medicine bring new rules. Staying informed is crucial.
2. Global Regulatory Variations
For companies operating across borders, handling different rules in each market can be time-consuming and complex. While some international bodies like the International Council for Harmonisation (ICH) work towards standardizing rules, significant differences remain.
3. Data Integrity and Security Risks
Pharmaceutical companies rely a lot on digital systems to handle clinical trials, manufacturing records, patient info, and reports for regulators. With cyber threats getting more advanced, keeping this data safe is very important.
Rules like 21 CFR Part 11 require companies to ensure that electronic data is secure, accurate, and cannot be changed without permission.
4. Managing Clinical Trial Compliance
Clinical trials are vital but come with strict oversight. Regulators expect companies to follow Good Clinical Practices (GCP) to ensure ethical trials, trustworthy data, and patient protection.
5. Resource and Expertise Limitations
Smaller businesses often struggle to maintain compliance because they lack large teams or budgets. It can be tough to keep up with rules in regions like the U.S. and EU without enough people or resources.
6. Cost of Compliance
Compliance isn’t cheap. Inspections, trials, and monitoring add up, especially for smaller organizations with fewer resources.
7. Ensuring Transparent and Accurate Labeling
Misleading or incomplete product labels can lead to major penalties. Labels must clearly state ingredients, dosage, usage instructions, side effects, and expiration dates.
Despite these hurdles, there are steps you can take to stay ahead.
Strategies for Effective Compliance Management
Compliance isn’t just a checkbox, it’s a mindset. The right systems and culture can make all the difference. Here’s how:
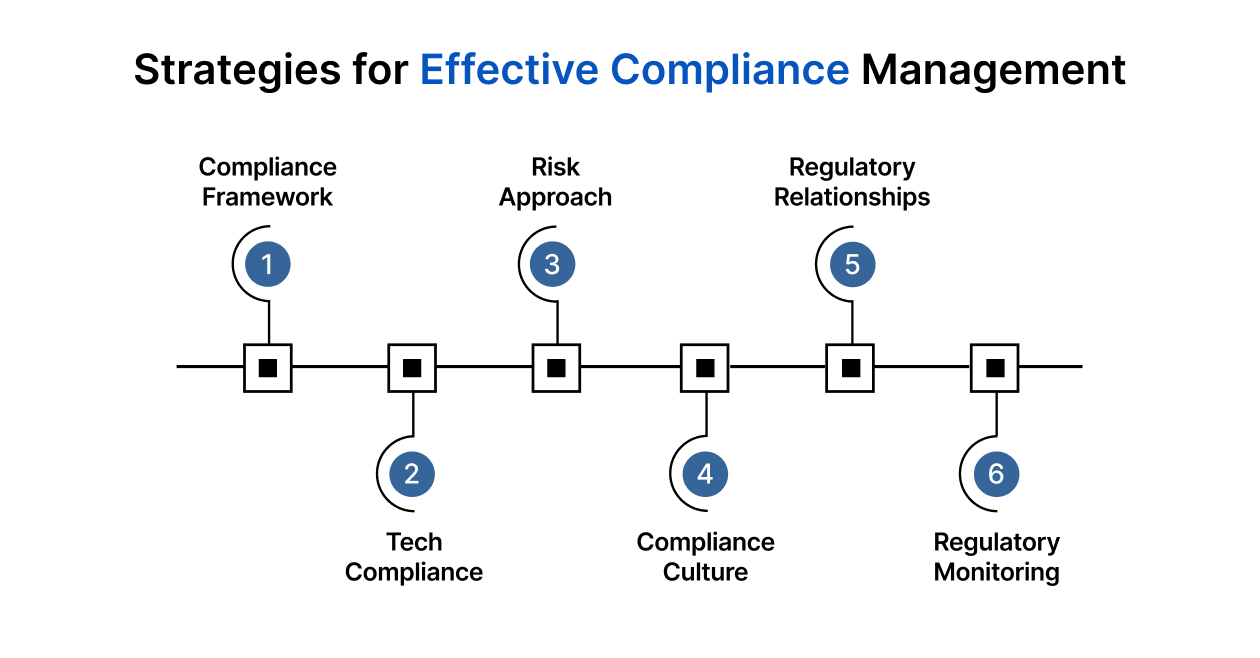
1. Implement a Dedicated Compliance Framework
Having a clear roadmap helps everyone stay aligned.
- Clear Guidelines: Clearly documented processes help meet FDA, EMA, or ICH standards.
- Defined Roles: Assigning tasks so everyone knows their responsibility.
- Internal Checks: Regular checks help catch and correct gaps before they become problems.
Having a dedicated framework lays the groundwork for managing complex regulations and reduces the risk of non-compliance.
2. Invest in Technology and Compliance Management Systems
Tools Technology can ease the compliance burden. Good tools help pharmaceutical companies:
- Automate Records: Automatically create and store documents to reduce manual errors.
- Track Regulatory Changes: Stay updated with the latest regulatory amendments in different regions, ensuring that all processes remain current.
- Keep Data Secure: Manage data to meet standards like 21 CFR Part 11 with clear records of every action.
Platforms like Atlas Compliance help track inspections, update regulatory changes, and prepare for audits—all from one place. This helps companies stay alert and audit-ready.
3. Develop a Risk-Based Approach
Not all risks are equal. Use a risk-based approach to stay focused. That includes:
- Risk Reviews: Regularly assess where issues are most likely to occur.
- Prioritize Efforts: Direct attention to areas that pose the greatest risk to patient safety or legal compliance.
- Action Plans: Putting systems in place to reduce those risks, like improving quality checks or oversight during trials.
This approach helps companies use time and resources where they’ll make the biggest difference.
4. Promote a Culture of Compliance
People play a big role in maintaining standards. That means:
- Staff Training: Keep staff updated on rules and procedures.
- Leadership Support: Senior leaders must champion compliance and back it with the right resources.
- Continuous Improvement: Encourage teams to find and fix weaknesses early.
When compliance becomes part of the company’s culture, employees are more engaged in following regulations, which lowers the chance of mistakes and oversights.
5. Establish Strong Relationships with Regulatory Authorities
Strong relationships with regulatory bodies can ease your compliance journey. This includes:
- Open Communication: Keep lines open throughout development and production.
- Early Engagement: Ask questions early to avoid surprises later.
- Regular Consultations: Join forums and discussions to stay current on updates.
Fostering a cooperative relationship with regulatory authorities can help you gain a clearer understanding of what is expected and avoid potential compliance issues in the future.
6. Monitor and Respond to Regulatory Changes
Compliance is a moving target. The more agile your systems, the easier it is to respond quickly. Key steps include:
- Staying Informed: Subscribe to updates, attend events, and engage with regulatory experts.
- Quick Adjustments: Update labels, adjust manufacturing steps, or revise documentation when needed.
By staying current with regulations, you can ensure that your products remain compliant throughout their lifecycle and avoid costly delays or penalties.
However, when operating across different countries, following the rules gets more complicated. Understanding international compliance and how countries work together helps make this easier. Let’s see how global standards affect pharmaceutical compliance.
International Compliance and Harmonization
Pharmaceutical companies often operate globally, facing different rules in each country. Because global regulations vary, international groups work to make them more consistent.
The ICH, for example, brings together regulators and industry experts to create shared guidelines. Adhering to these global standards offers several important benefits to both pharmaceutical companies and patients:
- Reduced Burden: Harmonized regulations reduce duplication of efforts for multinational companies.
- Faster Market Access: Drugs can be approved more quickly across multiple regions.
- Improved Safety: Consistent safety standards are applied worldwide.
- Cut Costs: Use the same paperwork in multiple markets.
Still, every company must watch for regional updates and adapt quickly to stay compliant and avoid delays in getting products approved.
Conclusion
Regulatory compliance in the pharmaceutical industry is essential for patient safety, product quality, and business success. While meeting these rules can be challenging, having the right strategies and tools makes it easier to stay on track and avoid costly mistakes.
Staying compliant doesn’t have to be a constant scramble. With the right tools, proactive planning, and a culture of accountability, you can build systems that not only meet regulations but stay ahead of them.
Let tools like Atlas Compliance make it easier to manage FDA inspections, stay on top of regulatory updates, and minimize risk, so your team can focus on what matters most: safe, effective medicine.
Looking to make compliance management easier and stay ready for inspections? Book a demo today and see how we can help your team work smarter and stay ahead.